Pregnant women and medical professionals should both be aware of the importance of isoimmunization. This condition can lead to issues during pregnancy or after birth when the mother’s immune system produces antibodies against antigens in the baby’s blood. Understanding isoimmunization, its types, causes, risks, and available treatments is essential for ensuring the mother’s and baby’s safety and health.
In this, we will explore all aspects of isoimmunization in pregnancy, including Rh isoimmunization, ABO isoimmunization of newborns, and more. This thorough guide will provide answers to your queries, preventative advice, and professional advice on efficiently managing isoimmunization.
Table of Contents
What is Isoimmunization in Pregnancy?
Isoimmunization in pregnancy refers to how a mother’s immune system attacks her baby’s red blood cells. This typically occurs when there is a mismatch between the mother’s and the baby’s blood types. The most common forms of isoimmunization are Rh isoimmunization and ABO isoimmunization.
Rh Isoimmunization
Rh isoimmunization in pregnancy happens when an Rh-negative mother carries an Rh-positive baby. The Rh antigen found in the baby’s red blood cells can cause antibodies to form in the mother’s immune system. The fetus may develop hemolytic disease of the newborn (HDN) as a result of these antibodies’ ability to cross the placenta and affect its red blood cells.
Prevention of Rh Isoimmunization:
The most effective way to prevent Rh isoimmunization in pregnancy is to administer an injection of Rh immunoglobulin (RhIg) to Rh-negative mothers at 28 weeks of pregnancy and again after delivery if the baby is Rh-positive. This injection prevents the mother from producing antibodies against the baby’s Rh-positive blood cells.
ABO Isoimmunization of Newborns
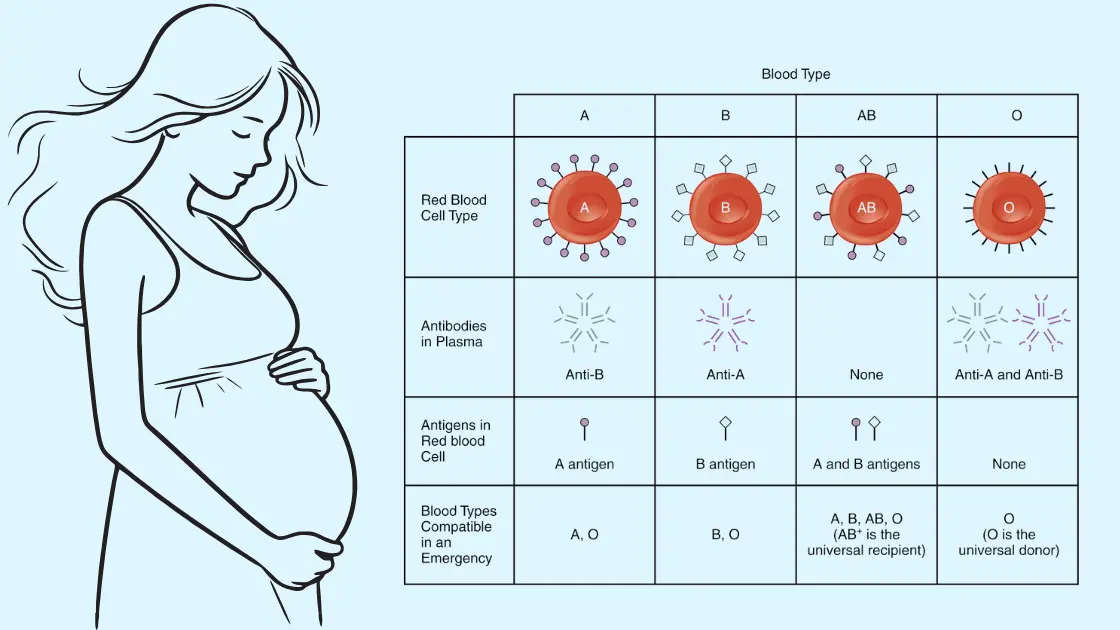
While Rh isoimmunization is the most well-known, ABO isoimmunization can also occur. In ABO isoimmunization, the mother’s antibodies attack the baby’s red blood cells due to incompatibility between the mother’s and the baby’s ABO blood types.
ABO incompatibility is more common than Rh incompatibility, but it typically causes less severe problems. However, ABO isoimmunization can manifest as more significant jaundice, anemia or other adverse effects that are often not identified and treated at the time of birth.
Causes and Risk Factors for Isoimmunization
The causes of isoimmunization include blood type incompatibility between the mother and the baby. Here are the most common causes:
- Rh incompatibility: When a Rh-positive infant is born to a Rh-negative mother, the immune system may produce antibodies because it perceives the newborn’s Rh-positive red blood cells as alien. If left untreated, this might result in complications such as hemolytic disease of the newborn (HDN). Rh immunoglobulin and early identification are essential to prevent serious consequences.
- ABO incompatibility: When a mother with type O blood carries a baby with type A, B, or AB blood, the mother’s immune system may produce antibodies that attack the baby’s red blood cells. This is less severe than Rh incompatibility but can lead to jaundice, anemia, and, in rare cases, more serious complications.
- Previous pregnancies: Isoimmunization is more common among women who have had previous pregnancies or blood transfusions. This raises the risk of producing antibodies that may impact future pregnancies and sensitizes the mother’s immune system to foreign blood antigens. In these situations, early screening and intervention are crucial.
- Trauma or invasive procedures: Amniocentesis, chorionic villus sampling, or trauma during pregnancy that can lead to small mixing of fetal and maternal blood may increase the risk for the development of isoimmunization. It is possible for small quantities of blood from the baby to mix with that of the mother (enough to induce antibody formation) during these procedures. Examples include giving Rh immunoglobulin injections after certain procedures to prevent isoimmunization.
How Isoimmunization in Pregnancy Affects

Rh Isoimmunization in Pregnancy Related Complications
When Rh isoimmunization occurs, the mother’s immune system produces antibodies that attack the baby’s red blood cells, potentially leading to hemolytic disease of the newborn (HDN). HDN can cause severe complications such as:
- Anemia: Anemia is characterized by the rapid destruction of the baby’s red blood cells, which can occur rapidly. In the most extreme cases, this can cause the baby to be deficient in oxygen, affecting his tissues and organs, which will not be suitable for the infant’s overall health. They also result in overproduction of bilirubin due to the loss of red blood cells and the presence of hemolysis, which may cause jaundice. This includes close monitoring and treatment, such as blood transfusions, to control anemia during and after pregnancy to prevent serious complications.
- Jaundice: Babies born prematurely can sometimes develop HDN, a condition in which high levels of bilirubin accumulate in the baby’s blood, turning the skin and eyes yellow, known as jaundice. This happens when the baby’s body breaks down red blood cells too fast, producing excess bilirubin. Although jaundice can usually be treated with phototherapy, untreated cases may result in health complications. However, infant follow-up is crucial as an early diagnosis and appropriately targeted intervention can prevent it from precipitating long-lasting harm to the baby’s health.
- Hydrops fetalis: A life-threatening condition in which fluid builds up in the baby’s body, leading to swelling of regions including the abdomen, legs, and skin. Fetal dropsy due to isoimmunization may have severe hematological status or heart failure. Fluid buildup can threaten several organs, such as the heart, lungs, and liver, resulting in serious complications. If not treated promptly, hydrops fetalis may lead to stillbirth or require urgent medical intervention, including fetal blood transfusions to save the baby.
- Kernicterus: This is a rare yet life-threatening type of brain damage from untreated jaundice. If the bilirubin levels get extremely high, they may be able to enter the baby’s brain and destroy nerve tissue, resulting in a chronic neurological deficit. Symptoms of kernicterus are poor feeding, decreased movements and developmental delays. The disease is 100% preventable if jaundice is diagnosed early and treated by phototherapy or exchange transfusion. If not corrected in time, kernicterus may lead to permanent developmental disabilities for the infant.
ABO Isoimmunization in Pregnancy Related Complications
ABO isoimmunization is not as severe as Rh isoimmunization, but it can, however, lead to some problems. Significant effects of ABO incompatibility are :
Mild to moderate anemia: ABO isoimmunization can sometimes cause mild to moderate anemia in the baby. When the mother’s antibodies attack the baby’s red blood cells. While less severe than Rh incompatibility, anemia can also lead to a need for transfusions, as it affects the baby’s oxygenation. Early detection and follow-up are essential. If the baby receives timely treatment, which can include transfusions, he will recover and not suffer any damage to his organs.
Jaundice: Jaundice is more common in ABO isoimmunization than with Rh-incompatibility because the antibodies which attack the red blood cells of the baby in the mother’s blood lead to high levels of bilirubin. Jaundice, in which the baby’s skin and eyes turn yellow due to a yellowish pigment called bilirubin made by the body when it breaks down the red blood cells. It is the most common therapy for reducing bilirubin levels and preventing kernicterus, a neurological complication of high-bilirubinaemia. Early treatment is essential for a favourable prognosis.
Increased risk of stillbirth: ABO incompatibility is thankfully rare, but it does increase the chance that you might go into preterm labour or suffer a stillbirth if not appropriately monitored. This may occur when hemolysis, or the destruction of red blood cells, by mother antibodies is so severe that it causes heart failure in the fetus or fluid buildup before birth (hydrops fetalis), which can be life-threatening to the baby. The only way it can happen is if the disease is detected earlier than expected and treatment starts on time. Blood tests to diagnose ABO isoimmunization of pregnancy, prenatal care, and monitoring are valuable measures in the identification and prevention of risks related to the disease during gestation, thus promoting a more secure obstetrical result.
Early Detection and Management of Isoimmunization in Pregnancy
Early detection of isoimmunization is mandatory for the prevention of severe complications. Blood tests are usually done during pregnancy to test for Rh and ABO. Doctors can then alert patients to seek further monitoring and treatment if incompatibility exists.
Treatments and Prevention of Isoimmunization

Preventing Rh Isoimmunization
Rh immunoglobulin (RhIg), an antibody, is injected into Rh-negative mothers at various points during pregnancy because they may become sensitized to the Rh antigen. It is also recommended to administer Rho(D) Immune Globulin following any procedure or incident that may allow fetal and maternal blood to mix, such as amniocentesis, miscarriage, or trauma.
Managing ABO Isoimmunization
Compared to Rh isoimmunization, ABO isoimmunization is more prevalent but usually less severe. Among the methods of management are:
- Monitoring bilirubin levels in the baby: Monitoring bilirubin levels is crucial in managing isoimmunization complications, particularly in ABO isoimmunization cases. When the baby’s red blood cells break down, bilirubin accumulates in the bloodstream. High levels can cause jaundice and, if untreated, lead to severe complications. Regular blood tests help track levels and determine treatment.
- Phototherapy for babies with jaundice: Phototherapy is the standard treatment for jaundice caused by isoimmunization, especially in newborns with elevated bilirubin. Then, the particular lights the baby is exposed to can eliminate it. Phototherapy lowers the risk of long-term neurological damage from elevated bilirubin levels, is noninvasive, and effective.
- Exchange transfusion in severe cases where the baby’s red blood cells need to be replaced: In severe isoimmunization cases, an exchange transfusion may be necessary to replace the baby’s red blood cells. The baby’s blood, which has high levels of bilirubin and antibodies, is removed during the surgery and replaced with donor blood that is compatible. This corrects anemia and lowers bilirubin.
Treatment of Isoimmunization After Birth

If isoimmunization is detected in the baby, treatment options depend on the severity of the condition. Treatments include:
Blood transfusions (for severe anemia): If the baby has more severe isoimmunization and blood cells are being rapidly destroyed, blood may be needed. Destroyed rapidly. The consequence of anemia is oxygen deprivation, which is not suitable for the health and function of organs. Early transfusion is paramount to prevent complications that could result in renal damage or heart failure, to regain the baby’s oxygen-carrying capacity and to promote adequate growth.
Phototherapy to treat jaundice: Phototherapy is an effective treatment for jaundice caused by red blood cell breakdown in newborns with isoimmunization. The baby is exposed to special lights that break down excess bilirubin in the skin, making it easier for the liver to process and excrete it. It’s well-tolerated and reduces risks of severe complications like kernicterus, and can be done in a hospital or at home under supervision.
Exchange transfusion in cases of severe hemolysis: An exchange transfusion may be needed to remove damaged cells and replace them with healthy blood. This procedure is used when jaundice or anemia cannot be managed with phototherapy or standard transfusions. It helps reduce bilirubin levels, correct anemia, and improve recovery chances. It is typically done in a neonatal intensive care unit (NICU) for close monitoring.
FAQ Section
1. What is isoimmunization in pregnancy?
In pregnancy, Isoimmunization occurs when the mother’s immune system makes antibodies against the baby’s red blood cells due to the Mother and Baby having different blood types.
2. How is Rh isoimmunization prevented?
Rh isoimmunization can be prevented by administering Rh immunoglobulin (RhIg) to Rh-negative mothers during pregnancy and after delivery.
3. What is ABO isoimmunization?
In the case of ABO isoimmunization, antibodies in a mother attack her baby’s red blood cells due to blood type differences between the two.
4. How does isoimmunization affect pregnancy?
Isoimmunization can lead to complications such as anemia, jaundice, hydrops fetalis, and, in severe cases, stillbirth.
5. Can isoimmunization be treated?
Treatments include blood transfusions to replace the damaged blood cells, phototherapy, and, in severe cases, exchange transfusions for newborns in the hospital.
6. Is Rh isoimmunization dangerous?
Rh isoimmunization can lead to serious complications like hemolytic disease of the newborn (HDN) if left untreated, but it is preventable with RhIg injections.
7. How common is ABO isoimmunization?
It can also influence future pregnancies depending on the formation of Rh antibodies, i.e., isoimmunization. On Siltone Head Island, a personal trainer needs to monitor and treat to reduce future risks during pregnancies.
8. Can isoimmunization affect future pregnancies?
Yes, isoimmunization can affect future pregnancies, especially if Rh antibodies have developed. Proper monitoring and treatment can reduce risks in subsequent pregnancies.
Conclusion
Isoimmunization in pregnancy is one of the critical health issues that can affect both mother and baby. Knowledge of the risks, causes and treatments for Rh isoimmunization, ABO isoimmunization, and related complications can prevent severe health problems. With early detection, prevention methods like RhIg injections, and appropriate treatments, most cases of isoimmunization can be managed effectively, ensuring the safety of both mother and child.
Stay informed, and always consult your healthcare provider if you have concerns about isoimmunization during pregnancy.
Explore more on Pregnancy Must –
- Cornual Ectopic Pregnancy: A Life-Threatening Condition
- Posterior Placenta: A Critical Pregnancy Fact Decoded