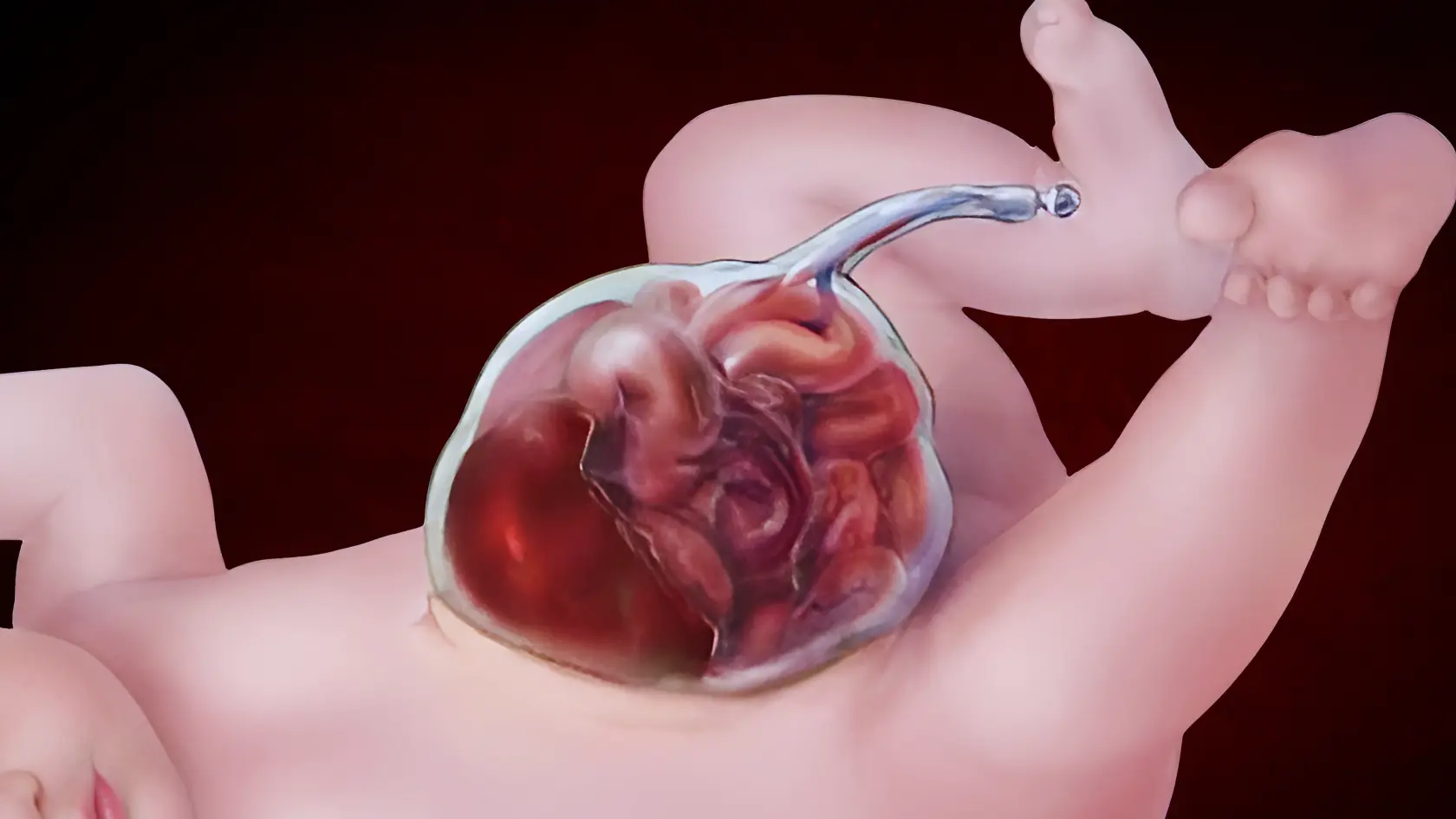
Exomphalos, or omphalocele, is a rare but serious birth defect that affects the abdominal wall of newborns. It happens when part of the baby’s intestines, liver, or other abdominal organs push through the belly button, usually inside a protective sac. This defect can vary in severity, and its effects can range from relatively minor issues to life-threatening complications. Understanding exomphalos in depth can help families and caregivers better prepare for treatment and care.
This pillar content will explain the definition, causes, symptoms, treatments, diagnosis methods (including exomphalos ultrasound), and real-life images of this birth defect. By the end, you’ll have a comprehensive understanding of this birth defect, including the answers to common questions.
What is Exomphalos? A Detailed Definition
Exomphalos is a congenital birth defect in which some of the baby’s abdominal organs, such as the intestines or liver, grow outside of the body through a hole in the abdominal wall, typically near the belly button. The protruding organs are often enclosed in a thin, transparent sac made up of the amniotic membrane. This condition is typically diagnosed during an ultrasound scan in the second trimester of pregnancy.
The severity of this birth defect varies widely. In some cases, only a small portion of the intestines or organs is outside the body, while in more severe cases, the entire liver or multiple organs may be outside the body. The condition is one of the more recognizable congenital birth defects and is generally treated with surgery.
Exomphalos vs. Gastroschisis
It’s important to distinguish exomphalos from another similar condition, gastroschisis, in which the intestines protrude from a hole in the abdominal wall but are not enclosed in a sac. While both conditions involve abdominal wall defects, the key difference is that exomphalos has the protective sac, which can sometimes offer some added protection to the organs.
Causes of Exomphalos
The exact cause of exomphalos is not always clear, but researchers have identified a few factors that may contribute to the occurrence of this birth defect.
Genetic Factors
There are some genetic disorders that are linked to high risk of exomphalos. As an illustration, one of the chromosomal abnormalities is trisomy 13 (Patau syndrome) and trisomy 18 (Edwards syndrome), which is known to greatly raise the chances of the baby being born with the defect. It also may be triggered by some genetic mutation, family inheritance pattern or hereditary syndrome like Beckwith-Wiedemann syndrome.
Environmental Factors
Along with genetic factors, environmental influences might play a role in the emergence of exomphalos. For instance:
- Maternal Smoking: Smoking during pregnancy increases the risk of birth defects, including exomphalos, by disrupting normal fetal development, decreasing blood flow to the placenta, and causing complications in organ formation.
- Exposure to Toxins or Chemicals: Environmental toxins, such as pesticides, pollutants, industrial chemicals, or even household cleaning products, can interfere with fetal development and increase the likelihood of birth defects, including exomphalos and other congenital conditions.
- Poor Maternal Nutrition: Inadequate nutrition during pregnancy, especially a lack of essential vitamins and minerals like folic acid, calcium, and iron, can impair fetal development and increase the risk of birth defects, including exomphalos. Proper prenatal nutrition is essential for the healthy formation of the baby.
- Certain Medications During Pregnancy: Certain drugs, particularly those not prescribed by a physician or self-administered without expert advice, would damage the growth of the fetus, interfere with the development of organs, and lead to diseases such as exomphalos. Never use any drug when pregnant, since certain drugs are known to be teratogenic.
These are both environmental and genetic factors, which can greatly contribute to the appearance of congenital defects, such as exomphalos, thus early prenatal care becomes extremely important in terms of reducing risks.
Developmental Issues
In fetal formation, the abdominal wall does not enclose the organs completely, resulting in exomphalos. The root cause of the organs coming out of the body is this failure to close in the initial stages of the pregnancy. Most exomphaloses are random, but certain environmental and genetic factors may affect the proper growth of the abdominal wall. Abnormal abdominal wall development can also be as a result of factors such as poor maternal health, infections or hormonal imbalances.
Symptoms and Diagnosis of Exomphalos
Exomphalos is mostly characterized by the prominent swelling or protrusion of internal organs in the belly button region that can be seen at birth. This protrusion is due to the bowel, liver, or other organs of the abdomen pushing out of the body. The size and severity of this bulge depend on how much of the organs are involved and whether the organs are enclosed in a protective sac. In more severe cases, the sac may rupture or be absent, leaving the organs exposed. This birth defect can be classified into small and large defects based on how much of the abdominal contents protrude.
Other possible symptoms that may occur alongside exomphalos include:
- Other congenital defects: These might affect other organ systems, such as the heart, lungs, or spine. In some cases, babies with exomphalos may also have heart defects or skeletal abnormalities, which can complicate the condition.
- Respiratory distress: If the protruding organs interfere with lung development or function, the baby may experience breathing difficulties at birth.
The intensity of the condition may be mild (small protrusion, few complications) or serious (large protrusion, multiple organ involvement, and other congenital defects). The existence of other malformations, including heart or neural tube defects, may have a major influence on the prognosis.
Though exomphalos is usually identified at birth, it is commonly also diagnosed before birth, which makes it possible to treat and provide care to the baby earlier. The disease is typically detected by ultrasound when a woman is pregnant, most of the time before the child is born, mostly between 18th and 22nd weeks.
Exomphalos Ultrasound Diagnosis

Exomphalos ultrasound is essential as a diagnostic measure, which is used to identify this birth defect in the prenatal stage. The ultrasound is normally conducted in the second trimester between the 18-22 weeks of pregnancy. This imaging device involves the use of sound waves to make an elaborate picture of the growing fetus in the womb which unveils defects in the belly of the fetus.
- The Ultrasound Process: The ultrasound technician will apply a gel to the mother’s abdomen and use a probe to send sound waves into the body. The sound waves bounce off the baby’s organs, and a computer creates an image. The image helps doctors assess the development of the fetus, including the presence of any abnormalities.
Key Aspects the Ultrasound Can Reveal:
- Size of the Defect: The ultrasound can help measure the extent of the abdominal wall defect, such as how much of the abdominal contents are outside the body. In small exomphalos, only a portion of the intestines may protrude, while large exomphalos may involve a significant portion of the abdominal organs.
- Presence of a Protective Sac: One of the defining features of exomphalos is whether the protruding organs are enclosed within a protective sac. In many cases, the organs are covered by a thin, transparent membrane. The presence of the sac offers some protection against infections and injury before birth, but if the sac is ruptured, the risk of complications increases. The ultrasound can help determine if the organs are protected or exposed.
- Associated Defects: In many cases of exomphalos, other congenital abnormalities may be present. The ultrasound can also help detect defects in the heart, spinal cord, kidneys, or limbs. For example, congenital heart defects are common in babies with exomphalos, and a detailed ultrasound can help identify these associated problems.
- Placental Health: The ultrasound may also assess how the placenta is positioned and whether there are any concerns about the placenta’s function, which could affect the baby’s development.
Additional Diagnostic Tests
If exomphalos is detected on an ultrasound, doctors may recommend additional tests to further assess the condition and look for any associated abnormalities. Some of the tests that may be performed include:
- Amniocentesis: This is a procedure in which a sample of the amniotic fluid surrounding the baby is taken using a needle inserted into the mother’s abdomen. The fluid has fetal cells in it that can be tested for chromosomal problems like trisomy 13 or trisomy 18. These genetic disorders increase the likelihood of exomphalos. Amniocentesis can also tell you a lot about the baby’s health in general and how likely it is that there will be other birth defects.
- Blood Tests: Maternal blood tests, such as the quad screen or serum alpha-fetoprotein (AFP) test, can be used to detect certain abnormalities and assess the risk of chromosomal conditions, although these tests are less definitive than amniocentesis.
- Magnetic Resonance Imaging (MRI): In some cases, a follow-up MRI may be recommended to get a clearer and more detailed view of the baby’s internal organs and any associated conditions that might not be fully visible on an ultrasound.
- Fetal Echocardiogram: If exomphalos is detected, and particularly if there are concerns about associated heart defects, a fetal echocardiogram (a specialized ultrasound of the heart) may be performed to assess the baby’s heart structure and function in more detail.
Early Detection and Planning for Treatment

Prenatal screening is very important for finding exomphalos early so that you can plan for the baby’s birth and medical care. If exomphalos is diagnosed, the healthcare team can get ready for the baby’s birth by making plans for surgery and other medical care that may be needed.
- Delivery Planning: Babies with exomphalos are often delivered in a specialized neonatal care unit where pediatric surgeons, neonatologists, and other specialists can provide immediate treatment. Early surgery is usually required to return the organs to the abdominal cavity and close the defect.
- Family Counseling: Families may also be offered counseling to help them understand the implications of the diagnosis, the treatment options, and the expected outcomes. Genetic counseling can also be an essential part of the process, especially if there is a risk of inherited conditions.
Exomphalos Treatment Options
After birth, the baby with exomphalos needs immediate care and a plan for surgery to fix the problem. How to fix the problem depends on how bad it is and if there are any other problems.
1. Surgical Repair
Surgical intervention is usually required to return the exposed organs to the abdominal cavity and repair the abdominal wall. Depending on the size of the protrusion and the number of organs involved, surgery may be done in one or multiple stages:
- Small Exomphalos: In cases where the defect is minor, involving only a small portion of the organs outside the body, surgery is usually performed soon after birth. This procedure is generally straightforward, with minimal complications. After surgery, the baby typically recovers quickly, and with proper care, the long-term outlook is often positive, allowing for normal development and health.
- Large Exomphalos: For more severe cases where multiple organs or larger portions of the abdomen are affected, surgery may be done in stages. This means that the organs are slowly put back into the abdomen over time, giving the abdominal cavity time to safely grow. This careful method lowers the chances of problems, puts less stress on the baby, and helps the baby get better more easily.
2. Post-Surgical Care and Recovery
After the surgical repair, the baby will need to be closely monitored for complications. These may include:
- Infections: There is a higher risk of infection because the internal organs are open to the outside world before surgery. Prompt surgical intervention, along with careful care and sterile techniques, can help lower this risk, but it is still a worry, especially for bigger defects where the exposed organs may be more likely to get sick and have problems.
- Respiratory Support: Babies with exomphalos may experience breathing difficulties, especially if there are other associated conditions, like lung issues or prematurity. In such cases, they may require additional respiratory support, such as oxygen therapy, a ventilator, or continuous positive airway pressure (CPAP) to help them breathe properly and ensure their lungs receive sufficient oxygen while they stabilize.
- Nutritional Support: Due to the surgical repair and potential difficulties with feeding, babies may need to be nourished through a tube or IV initially. As they recover from surgery, their digestive system may need time to adapt, and they may gradually transition to oral feeding once their condition stabilizes and they show the ability to handle nutrition properly.
3. Long-Term Outlook
Many children who undergo successful surgery for exomphalos go on to live healthy lives. However, long-term follow-up care is often necessary to check for complications like developmental delays or growth issues. Regular check-ups with pediatricians and specialists are recommended to monitor overall health and development.
Can Exomphalos Be Prevented?

Currently, there is no guaranteed way to prevent exomphalos, as most cases occur randomly during pregnancy. However, there are steps that can reduce the likelihood of birth defects in general:
- Prenatal Care: It’s very important to see a doctor regularly during pregnancy to look for possible birth defects early on. Early screenings, ultrasounds, and blood tests can help find problems like exomphalos and other birth defects. This lets doctors treat them right away, which is better for both the mother and the baby.
- Healthy Lifestyle Choices: To lower the risk of birth defects, it’s important to live a healthy lifestyle by not smoking, drinking too much, and taking important prenatal vitamins like folic acid. A healthy pregnancy and baby can also be helped by eating a balanced diet, staying active, getting enough sleep, and keeping stress levels low.
Genetic Counseling: If there is a family history of birth defects or conditions like exomphalos, genetic counseling can provide insight into the risks for future pregnancies. This lets couples make smart choices about family planning, possible screenings, and ways to keep their child from getting sick, all while knowing how likely it is that their child will inherit a condition.
Frequently Asked Questions About Exomphalos
1. What is the survival rate for babies with exomphalos?
The survival rate for babies with exomphalos has greatly improved due to advances in neonatal care and surgical techniques. However, the survival rate depends on the severity of the condition and any other associated birth defects.
2. How is exomphalos treated?
Exomphalos typically requires surgery to place the protruding organs back inside the abdominal cavity and close the defect. After surgery, babies may need additional support, including respiratory or nutritional assistance.
3. Can exomphalos be detected before birth?
Yes, exomphalos is usually detected through a prenatal ultrasound, often between 18 and 22 weeks of pregnancy. The condition may be confirmed with additional tests like amniocentesis if needed.
4. What are the long-term effects of exomphalos?
Depending on how bad the condition is, the long-term effects of exomphalos can be different. Some kids have problems with growth or development, but many go on to live healthy, active lives after surgery and medical care.
5. Is exomphalos genetic?
While some genetic conditions are associated with exomphalos, such as trisomy 13 or trisomy 18, most cases occur randomly, without a family history of the condition.
By understanding the details of exomphalos, its causes, treatment options, and the possible outcomes, families can better navigate this challenging condition. With the right medical care and emotional support, many children with exomphalos go on to live healthy and fulfilling lives.
Explore more on Pregnancy Must –